The Affordable Care Act (ACA), also known as Obamacare, is a U.S. healthcare reform law enacted in 2010 under President Barack Obama. It aimed to increase access to affordable health insurance, reduce healthcare costs, and expand Medicaid. The ACA introduced health insurance marketplaces, mandated essential health benefits, and prohibited insurance discrimination based on pre-existing conditions.
The law also included the individual mandate, requiring most Americans to have health insurance or pay a penalty (which was eliminated in 2019). Businesses with 50+ full-time employees must provide health coverage under the employer mandate.
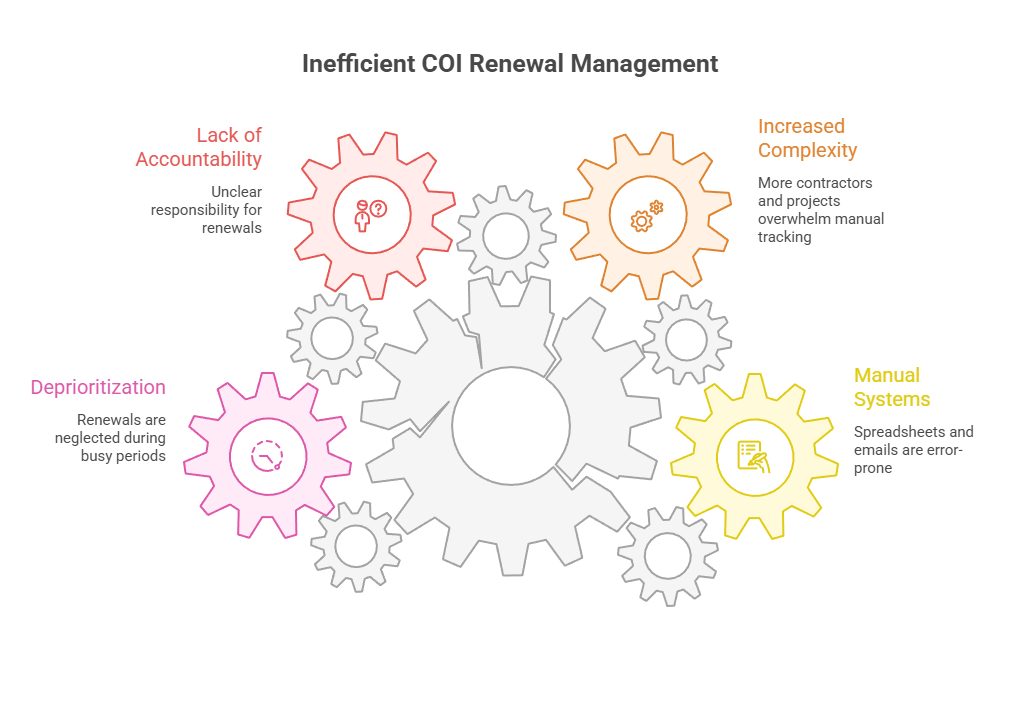
Simplify credential management
Tracking employee certifications and licenses doesn't have to be complicated. Expiration Reminder helps you send automated notification and keep your company compliant.

Key Facts
- Major Goals of the ACA:
- Expanded Health Insurance Coverage: Created state and federal marketplaces for people to buy subsidized health insurance.
- Improve Healthcare Quality: Mandated essential health benefits like preventive care, maternity care, and mental health services.
- Protect Consumers: Stopped insurers from denying coverage for pre-existing conditions or charging higher rates based on health status.
- Key Provisions of the ACA:
- Pre-Existing Conditions Protection: Insurance companies cannot deny coverage or charge higher premiums for people with pre-existing conditions.
- Health Insurance Marketplaces: Allows individuals to purchase coverage with government subsidies based on income.
- Medicaid Expansion: Allowed states to expand Medicaid eligibility (not all states adopted this, however).
- Employer Mandate: Requires businesses with 50+ full-time employees to offer health insurance or face penalties.
- Young Adult Coverage: Allows children to stay on their parents' insurance plans until age 26.
- Essential Health Benefits: Requires all ACA-compliant plans to cover services like preventive care, hospitalization, prescription drugs, and mental health services.
- Impact of the ACA:
- Over 20 million Americans gained health insurance.
- The uninsured rate dropped significantly, especially among low-income individuals.
- Healthcare costs slowed in growth, though some premiums increased in certain markets.
- Changes and Challenges:
- In 2017, the individual mandate penalty was reduced to $0 under the Tax Cuts and Jobs Act.
- Several lawsuits and political efforts have attempted to repeal or weaken the ACA.
- Some states expanded Medicaid, while others did not, creating coverage gaps in certain regions.
1. What is the Affordable Care Act (ACA) and why was it created?
The Affordable Care Act (ACA), often referred to as Obamacare, is a comprehensive healthcare reform law passed in the United States in 2010 under the administration of President Barack Obama. The primary goal of the ACA was to expand access to healthcare, make healthcare more affordable, and improve the quality of care provided to individuals across the U.S. It aimed to achieve these goals through a variety of measures, including expanding insurance coverage, regulating the health insurance market, and promoting preventative care.
Key Goals of the Affordable Care Act
- Expanding Healthcare Access
- One of the ACA's core objectives was to make healthcare accessible to more Americans. It sought to achieve this by expanding Medicaid, providing subsidies to lower-income individuals, and creating a state-based health insurance marketplaces (also called exchanges) where individuals and small businesses could purchase insurance.
- The ACA aimed to reduce the number of uninsured Americans by offering a range of options for individuals who might not otherwise have been able to afford insurance.
- Making Healthcare More Affordable
- The ACA introduced measures to lower the cost of healthcare, such as offering subsidies to help individuals with lower incomes purchase health insurance, expanding Medicaid in many states, and regulating premium rates charged by insurance companies.
- It also sought to improve the efficiency of healthcare delivery, encouraging preventive care and the use of value-based care rather than a free-for-service model, which had often incentivized overuse of healthcare services.
- Improving Healthcare Quality
- The ACA focused on improving the quality of care by implementing measures aimed at reducing medical errors, promoting the use of electronic health records, and requiring health insurers to spend a certain percentage of premiums on patient care.
- It also introduced preventive health services with no out-of-pocket costs for policyholders, encouraging regular check-ups, screenings, and vaccinations to prevent chronic illnesses.
- Reform of the Health Insurance Market
- The ACA introduced a set of regulations for the health insurance industry to make coverage more equitable. For example, it prohibited denying coverage due to pre-existing conditions, ensured that insurance premiums would not be based on gender or health status, and created minimum coverage standards for all health plans.
- It also required most large employers (those with 50 or more full-time employees) to offer health insurance to their workers or face a penalty. This aimed to ensure that employers contribute to the healthcare needs of their employees.
Why Was the Affordable Care Act Created
The ACA was created in response to several key problems and challenges within the U.S. healthcare system:
- High Number of Uninsured Americans
Before the ACA, millions of Americans were without health insurance, either because they couldn't afford it or because they didn't qualify for employer-sponsored coverage or government assistance. The high uninsured rate led to inadequate access to medical care, financial strain for individuals who needed healthcare but couldn't afford it, and higher rates of preventable diseases and mortality.
- Rising Healthcare Costs
Healthcare costs in the U.S had been rising at an unsustainable rate, making it increasingly difficult for families, businesses, and the government to afford coverage. Health insurance premiums and out-of-pocket costs (like deductibles and co-pays) were rising faster than inflation or wage, putting healthcare out of reach for many people. The ACA sought to reduce healthcare spending by improving the efficiency of the healthcare system and promoting preventive care, which could ultimately reduce long-term costs associated with chronic diseases.
- Inefficiencies in the Healthcare System
Prior to the ACA, there was significant fragmentation in the healthcare system. Many Americans had limited access to care or faced substantial barriers to getting the treatment they needed. Some groups, such as individuals with pre-existing conditions, were often unable to find affordable insurance. The ACA sought to address these inefficiencies by increasing transparency in the insurance market, expanding access to coverage, and setting minimum standards for insurance policies, ensuring that individuals would not be left without coverage due to their health status or other factors.
- Healthcare Disparities
The ACA was also created to address health disparities by ensuring that vulnerable populations - such as low-income individuals, racial minorities, and people living in rural areas - had greater access to quality healthcare. Expanding Medicaid eligibility to more low-income individuals and offering healthcare subsidies were key provisions aimed at reducing disparities in health access and outcomes across different socioeconomic groups.
- Healthcare System Reform
There was a broad push to reform the U.S. healthcare system, which was the most expensive in the world but faced challenges with access, efficiency, and quality. The ACA aimed to provide a more comprehensive approach to reform, focusing on cost control, access to care, quality improvements, and health outcomes.
Key Provisions of the ACA
- Health Insurance Marketplaces: The ACA created state-based or federal health insurance marketplaces where individuals could compare and purchase health insurance plans. These marketplaces were designed to make it easier to shop for coverage and help individuals find affordable options, with a focus on those who did not have employer-sponsored insurance.
- Medicaid Expansion: The ACA allowed states to expand Medicaid to cover more low-income individuals, with the federal government covering the majority of the cost for the expansion. As of 2025, not all states have expanded Medicaid, leading to coverage gaps in certain regions.
- Subsidies for Low-Income Individuals: The ACA provided subsidies for people with incomes between 100% and 400% of the federal poverty level to help them purchase insurance on the marketplaces. These subsidies were designed to make health insurance more affordable for middle and lower-income individuals and families.
- Pre-existing Conditions and Coverage Requirements: The ACA prohibited health insurers from denying coverage based on pre-existing conditions, ensuring that people with chronic or prior health issues could not be excluded from coverage. The ACA also established essential health benefits, requiring insurers to cover services like maternity care, mental health services, prescription drugs, and preventive services.
- Individual Mandate: The ACA initially included an individual mandate requiring most Americans to have health insurance or face a penalty, though the penalty was effectively eliminated in 2019 for most individuals through changes made in the Tax Cuts and Job Act 0f 2017.
- Employer Mandate: The ACA also included an employer mandate, requiring large employers (those with 50 or more full-time employees) to provide health insurance to their employees or pay a penalty.
In conclusion, the ACA was created to address the significant challenges within the U.S. healthcare system, including the high number of uninsured individuals, rising healthcare costs, inefficiencies, and health disparities. By expanding access to insurance, improving quality, and controlling costs, the ACA aimed to create a more equitable, affordable, and efficient healthcare system for Americans. While the ACA has faced significant political challenges and revisions since its passage, it remains a landmark piece of legislation with enduring effects on healthcare in the U.S.
2. Is health insurance required under the ACA?
Under the Affordable Care Act (ACA), health insurance was initially required for most Americans, but the individual mandate that enforced this requirement has been effectively eliminated for most individuals. Below is an overview of how health insurance requirements have evolved under the ACA:
- The Individual Mandate (Before 2019)
- Original Requirement: The ACA initially included a provision known as the individual mandate, which required most Americans to have health insurance or face a penalty. The goal of this mandate was to ensure that more people participated in the insurance market, thus lowering the overall cost of health insurance by spreading the risk across a larger pool of people.
- Penalty for Non-Compliance: If someone did not have health insurance and did not qualify for an exemption, they were required to pay a penalty when filing their federal taxes. This penalty was calculated as either a fixed amount or a percentage of household income (whichever was higher).
- The Elimination of the Penalty (2019)
- Tax Cuts and Jobs Act of 2017: In December 2019, the Tax Cuts and Jobs Act was passed, which effectively eliminated the individual mandate penalty starting in 2019. This means that individuals who do not have health insurance are no longer subject to a penalty for failing to comply with the mandate, with one key exception:
- California, Massachusetts, New Jersey, Rhode Island, and Washington D.C. have enacted their own state-level individual mandates that still require residents to have health insurance or pay a penalty. These states have continued to enforce their own penalties for non-compliance, even though the federal mandate was replaced.
For most Americans, the ACA no longer requires health insurance, since the federal penalty was eliminated in 2019. However, as mentioned, some states have enacted their own individual mandates with penalties for not having coverage. These states require their residents to have health insurance or face a state-level penalty.
Why was the Individual Mandate Eliminated
- Political and Legal Factors: The individual mandate became one of the most controversial aspects of the ACA. Many people opposed it, arguing that it infringed on personal freedoms by forcing people to purchase health insurance. The repeal of the penalty was part of broader political negotiations and legal challenges related to the ACA.
- Impact on the Market: Supporters of the individual mandate argued that it was crucial for maintaining a stable and affordable health insurance market by ensuring that healthy individuals also enrolled in coverage, thus helping to balance the risk pool. With the elimination of the penalty, there were concerns about rising premiums and a potential increase in the number of uninsured Americans, particularly among healthier populations.
Health Insurance and Marketplace and Subsidies
While the individual mandate penalty is no longer in place for most Americans, the health insurance marketplaces created under the ACA remain active, and subsidies to help lower-income individuals afford coverage are still available. These subsidies are provided to individuals and families whose incomes fall between 100% and 400% of the federal poverty level, helping them purchase health insurance through the Health Insurance Marketplace.
These subsidies can make healthcare coverage more affordable for individuals, even if they are not required to purchase it under the law. The open enrollment periods for purchasing insurance on the marketplace are also still in place, though there are special enrollment periods for individuals who experience certain life events, such as marriage, birth of a child, or loss of job-based coverage.
Exemptions to the Requirement
Even under the original ACA mandate, there were certain exemptions from the requirement to have health insurance. Examples can include:
- Financial Hardship: People who could not afford health insurance based on their income.
- Religious Beliefs: People who objected to having health insurance due to their religious beliefs.
- Short Coverage Gaps: Individuals who went without insurance for less than three months.
- Other Special Circumstances: Such as being incarcerated, ineligible for Medicaid, or living outside the country for a certain period of time.
3. How does the ACA help people in low income?
The Affordable Care Act (ACA) provides significant support for individuals and families with low income by increasing access to affordable health insurance, expanding coverage options, and offering financial assistance. Some ways in which the ACA helps people with low income include:
- Expansion of Medicaid
One of the ACA's most impactful provisions was the expansion of Medicaid. Medicaid is a joint federal and state program that provides health coverage to low-income individuals and families. Before the ACA, Medicaid eligibility was more limited, and many low-income adults, particularly those without children, did not qualify. The ACA allowed states to expand Medicaid to include all adults with incomes up to 138% of the federal poverty level, regardless of whether they have children or other qualifying conditions. In states that chose to expand Medicaid, it provided free or low-cost health coverage to millions of low-income individuals. However, not all states have expanded Medicaid - 12 still remain, leaving many low-income individuals int these states without access to affordable health insurance.
- Subsidies for Health Insurance on the Marketplace
Health Insurance Marketplaces (also known as exchanges) were created by the ACA to help individuals purchase health insurance, particularly for those who do not have access to employer-sponsored coverage. For people with low to moderate incomes, the ACA provides subsidies to help make insurance premiums and out-of-pocket costs more affordable.
For people whose income is between 100% and 400% of the federal poverty level, the ACA provides premium tax credits that reduce the cost of monthly insurance premiums. These subsidies are designed to ensure that health insurance is affordable for people who may not be able to afford the full premium price. For individuals with incomes between 100% and 250% of the federal poverty level, the ACA also provides cost-sharing reductions. These reductions lower the amount of money individuals have to pay out-of-pocket for deductibles, co-pays, and co-insurance.
- Preventive Care with No Out-of-Pocket Costs
The ACA requires that most insurance plans cover a variety of preventive health services without charging any out-of-pocket costs (such as co-pays or deductibles). These services include things like:
- Vaccines
- Cancer screenings (mammograms, colonoscopies, and more)
- Routine wellness visits
- Contraception and prenatal care
This is especially helpful for people with low income because it encourages regular check-ups and preventive care, which can prevent more serious and costly health problems down the road.
- No Denial for Pre-existing Conditions
Before the ACA, individuals with pre-existing conditions (such as diabetes and heart disease) often faced discrimination or were denied coverage by insurance companies, especially if they had low incomes. The ACA prohibits insurers from denying coverage or charging higher premiums to people based on pre-existing conditions. This provision ensures that people with chronic health conditions can get the care they need without being financially burdened, making health insurance more accessible and affordable.
- Affordability and Health Coverage
The ACA established health insurance marketplaces where low-income individuals and families can compare and purchase health plans. These plans are categorized into four tiers - Bronze, Silver, Gold, and Platinum - based on how much the plan covers versus how much the individual is responsible for paying out of pocket. The Silver Plan is particularly helpful for individuals who qualify for cost-sharing reductions, making the insurance plan more affordable. These plans help low-income families avoid the high costs of care while ensuring that they receive adequate coverage for their medical needs.
- Young Adults and Dependent Coverage
The ACA allows young adults under the age of 26 to stay on their parent’s health insurance plan. This provision helps low-income families, particularly those who have recently graduated from school or are starting their careers, by allowing them to maintain coverage until they can secure their own. This is particularly important for young adults who may not have employer-sponsored insurance or the financial resources to purchase health coverage on their own.
- Protection Against Health Insurance Scams and Unfair Practices
The ACA introduced regulations to protect consumers from unfair practices by insurance companies. For example, insurance companies can no longer:
- Set annual or lifetime limits on coverage.
- Drop coverage when an individual gets sick or files a claim (known as "rescission").
- Engage in discriminatory pricing based on gender or health status.
These protections ensure that people with low incomes are not taken advantage of by the insurance industry and can get the care they need without fear of financial ruin.
- Expansion of Community Health Centers
The ACA provided funding for community health centers, which are crucial for providing primary care to low-income and underserved populations. These centers offer a wide range of medical services, often on a sliding fee scale based on income. This helps ensure that low-income individuals have access to affordable care, regardless of their ability to pay.
These provisions make health care more accessible and affordable for individuals and families with low income, ensuring that they have the opportunity to lead healthier lives without facing financial hardship due to medical costs.
4. What are the essential health benefits required under the ACA?
Under the Affordable Care Act (ACA), health insurance plans offered in the individual and small group markets (including those purchased through the Health Insurance Marketplace) are required to cover 10 essential health benefits. These benefits are designed to ensure that all Americans have access to comprehensive, affordable, and essential healthcare services, regardless of their health status or income. The 10 essential health benefits (EHBs) that must be covered by health insurance plans under the ACA encompass:
- Ambulatory Patient Services (Outpatient Care): This includes care you receive outside of a hospital, covering services such as routine doctor visits, outpatient surgery, diagnostic tests, and specialist care (physical therapy or mental health counseling) that do not require an overnight stay in a hospital.
- Emergency Services: Emergency care must be covered regardless of whether the healthcare provider is in-network or out-of-network. This includes services related to medical emergencies, such as ambulance rides, emergency room visits, and urgent care for serious conditions like heart attacks, strokes, or broken bones.
- Hospitalization: Hospital stays must be covered under the ACA. This includes inpatient care for surgeries, overnight stays in the hospital, treatment for serious illnesses, childbirth, and rehabilitation following a major health event.
- Maternity and Newborn Care: Plans must cover maternity care (for example, prenatal and postnatal care) and newborn care (such as medical services for newborns immediately after birth). This ensures that women can receive comprehensive care throughout pregnancy and that newborns receive the necessary medical services right from birth.
- Mental Health and Substance Use Disorder Services: Mental health services and substance use disorder treatment must be covered. This includes therapy and counseling, inpatient treatment for mental health conditions, and outpatient care for substance abuse disorders. The ACA requires that mental health services be covered at parity with medical and surgical benefits, meaning that they cannot be subject to more restrictive coverage rules than those applied to other types of care.
- Prescription Drugs: Health plans must cover a range of prescription medications. This includes drugs needed to treat chronic conditions (such as insulin for diabetes, blood pressure medications), as well as medications required to manage short-term conditions (such as antibiotics for infections). Plans are required to include a drug formulary, or list, of covered drugs, though the specific drugs covered may vary by plan.
- Rehabilitative and Habilitative Services and Devices: This category includes both rehabilitative services (for example, physical therapy to recover from surgery or injury) and habilitative services (for example, speech therapy or occupational therapy to help individuals with disabilities improve their abilities). Rehabilitative devices might include things like wheelchairs or prosthetics.
- Laboratory Services: Plans must cover laboratory tests such as blood tests, urine tests, X-rays, and diagnostic screenings to diagnose conditions, monitor health conditions, and detect diseases. This category ensures that individuals have access to necessary diagnostic services.
- Preventive and Wellness Services and Chronic Disease Management: The ACA mandates that health plans cover a wide range of preventive services without cost-sharing (no co-pays, co-insurance, or deductibles). This includes services like:
- Vaccinations (such as flu shots, childhood immunizations)
- Screenings for cancer (mammograms, colonoscopies, and more), cholesterol, diabetes, and other conditions
- Counseling for smoking cessation, weight management, and other health-promoting behaviors
- Wellness visits, such as annual check-ups and health screenings
- Chronic disease management services to help individuals manage long-term health conditions like diabetes, hypertension, and asthma.
- Pediatric Services, Including Oral and Vision Care: Pediatric services must be covered for children under the age of 19. This includes regular well-child visits, vaccinations, and screenings. Additionally, oral care (dental check-ups, cleanings, fillings) and vision care (eye exams, glasses, and contact lenses) must be included for children.
Important Notes
- The essential health benefits are required to be included in all individual and small group health plans, including those offered through the Health Insurance Marketplace.
- Large employer health plans (for employers with 50 or more full-time employees) are not required to offer all of these benefits, although many do, particularly when they are offered through the Marketplace.
- While the ACA mandates the coverage of these essential benefits, the specifics of coverage (such as the types of prescription drugs or specific mental health services covered) may vary depending on the health plan.
These benefits were designed to ensure that health insurance coverage provides comprehensive care and addresses the essential health needs of individuals, including preventive care, mental health, chronic disease management, and emergency services. By requiring these services, the ACA aims to improve access to necessary care, prevent health issues from becoming more serious, and help reduce healthcare disparities.
5. How did the ACA change employer health insurance requirements?
The Affordable Care Act (ACA) introduced significant changes to the health insurance requirements for employers, particularly for large employers. These changes were designed to improve access to affordable health insurance for employees and to incentivize employers to offer coverage. Key ways the ACA changed employer health insurance requirements include:
- Employer Mandate (The Employer Shared Responsibility Provisions)
- The ACA’s employer mandate requires large employers (with 50 or more full-time employees or the equivalent in part-time employees) to either:
- Provide affordable health insurance that meets the ACA’s standards to their full-time employees, or
- Pay a penalty if they fail to do so.
- Full-time employees are defined as employees who work 30 or more hours per week.
- Affordable coverage is defined as coverage that costs the employee no more than 9.83% of their household income for the employee's share of the premium in 2021. The plan must also provide a minimum value, meaning the plan must cover at least 60% of the total cost of medical services.
- Employer Penalty for Non-Compliance: If an employer does not provide affordable coverage to full-time employees and at least one employee qualifies for premium tax credits to purchase insurance through the Health Insurance Marketplace, the employer may face a penalty.
- Penalties: The penalties are assessed annually, and they can be quite large. For example, in 2021, the penalty for not offering coverage at all was $2,700 per employee (with a first 30 employees excluded), and the penalty for offering coverage that is not affordable or does not meet the minimum value was about $4,060 per employee who receives a subsidy for marketplace coverage.
- Health Insurance Marketplace (SHOP) for Small Employers
- For small employers with fewer than 50 full-time employees, the ACA created the Small Business Health Options Program (SHOP) to help businesses offer health insurance to their employees. The SHOP marketplace allows small businesses to provide coverage options for employees and may also provide tax credits to help reduce the cost of coverage.
- Small businesses with fewer than 25 employees and average annual wages of $50,000 or less may qualify for a tax credit to help offset the cost of providing insurance through the SHOP marketplace.
- Essential Health Benefits Requirement
- Under the ACA, health plans provided by employers must include coverage for the 10 essential health benefits (EHBs) if they are offered in the individual or small group market. This includes services like preventive care, emergency services, maternity care, mental health services, and prescription drugs.
- However, large employers offering self-insured plans may have some flexibility in how they structure their benefits, though they still need to comply with minimum value requirements (such as covering at least 60% of the cost of healthcare services).
- Prohibition of Pre-Existing Condition Exclusions
- The ACA banned discrimination based on pre-existing conditions. This means that employers cannot deny health insurance coverage or charge higher premiums to employees or their family members based on health conditions they had before enrolling in the plan. This provision applies to all employers offering health insurance, regardless of size.
- Elimination of Annual and Lifetime Limits
- The ACA prohibited health insurance plans from imposing annual or lifetime limits on essential health benefits. This ensures that employees with serious or chronic health conditions do not face financial barriers to necessary care once they reach a limit on their health benefits.
- Health Insurance Coverage for Dependents
- Under the ACA, employer-sponsored health plans are required to allow young adults to remain on their parents' health insurance plan until the age of 26. This provision applies to all employer health plans, regardless of the size of the employer, and helps young adults who may not have access to their own employer-sponsored coverage or who are just entering the workforce.
- Reporting and Disclosure Requirements
- The ACA introduced new reporting and disclosure requirements for employers. Specifically, employers with 50 or more full-time employees are required to report to the Internal Revenue Service (IRS) and to employees about the health insurance they offer, including:
- Whether they offer health insurance coverage.
- The cost of the coverage.
- The minimum value of the coverage.
- The employee’s eligibility for subsidies through the Health Insurance Marketplace.
- Employers are required to file Forms 1095-C and 1094-C with the IRS and provide employees with a Form 1095-C that details their health insurance coverage for the year. This reporting is essential for ensuring compliance with the ACA’s employer mandate.
- Wellness Programs
- The ACA encouraged the implementation of wellness programs that provide employees with access to preventive care, health screenings, and other services that promote healthy lifestyles.
- It also regulated wellness programs to ensure they are not discriminatory. For example, employers may offer discounts on premiums or other incentives for participation in wellness programs, but the ACA limits the amount of the reward to 30% of the cost of coverage (up to 50% for programs focused on tobacco cessation).
- Cost Control and Transparency
- The ACA also introduced measures to control health care costs for employers and employees. For example, the ACA required insurance companies to justify premium increases above 10% for individual and small group plans.
- Employers must also provide clear information about insurance coverage, making it easier for employees to understand the details of their plan, what it covers, and the costs associated with it.
- Automatic Enrollment (For Large Employers)
- Though it was intended to be implemented, the ACA includes provisions for automatic enrollment in employer-sponsored health insurance for large employers (those with 200 or more employees). This provision would require employers to automatically enroll employees in the company’s health plan if they did not choose a plan themselves. However, this provision has been delayed indefinitely, and employers are not currently required to implement automatic enrollment.
Summary of Key Changes in Employer Health Insurance Requirements
- Employer Mandate: Large employers (50+ full-time employees) must offer affordable health insurance or face penalties.
- Health Insurance Marketplace: Small employers can offer insurance through the SHOP marketplace and qualify for tax credits.
- Essential Health Benefits: Employer plans must cover the ACA’s 10 essential health benefits.
- Pre-existing Conditions: Employers cannot exclude individuals from coverage or charge higher premiums based on pre-existing conditions.
- No Lifetime/Annual Limits: Employer health plans cannot impose lifetime or annual limits on essential health benefits.
- Dependent Coverage: Employees can keep young adults (up to age 26) on their health insurance plans.
- Reporting Requirements: Employers must report to the IRS about the insurance they provide, including employee eligibility for subsidies.
- Wellness Programs: Employers are encouraged to implement wellness programs with limited rewards or penalties.
- Cost Control and Transparency: The ACA imposes measures to control insurance premiums and promote transparency in coverage.
- Automatic Enrollment: Large employers are required to implement automatic enrollment (though delayed).
The ACA significantly altered the landscape of employer-provided health insurance, with a focus on increasing access to affordable coverage, promoting transparency, and eliminating discrimination. The goal was to ensure that employers provide meaningful health coverage to their workers while reducing the number of uninsured individuals.
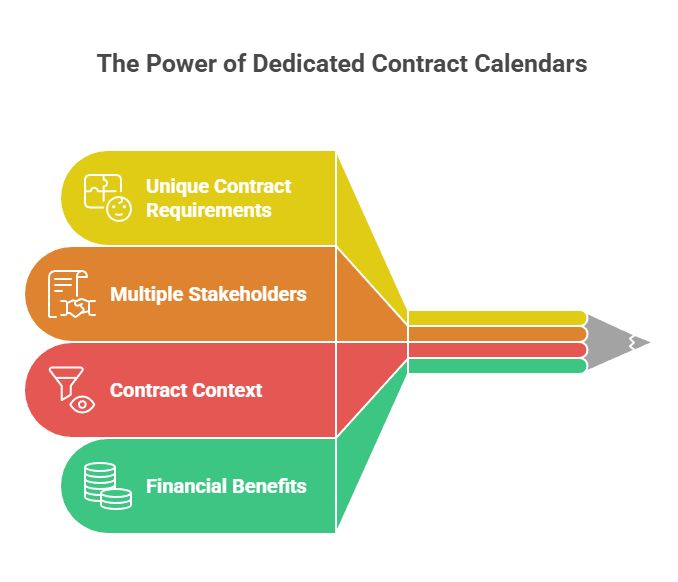
Make sure your company is compliant
Say goodbye to outdated spreadsheets and hello to centralized credential management. Avoid fines and late penalties by managing your employee certifications with Expiration Reminder.