Table of Contents
Imagine it’s November in a busy hospital. Flu season is ramping up, and one unvaccinated nurse catches influenza. Within days, a handful of patients and staff members fall ill. As an HR manager, you’re scrambling: could this have been prevented? Scenes like this are precisely why many healthcare organizations require annual flu vaccinations for their workers. In this post, we’ll discuss why those yearly flu shots matter, what the data shows, how mandates have worked out, the challenges hospitals faced (and solved), and how tools like Expiration Reminder make managing it all easier. Grab a coffee and let’s dive in!
Why Do Healthcare Workers Need Flu Vaccines Every Year?
Getting a flu shot every year can feel routine – but there’s solid reasoning behind it. Influenza viruses change constantly, so last year’s shot won’t fully protect you this year. Immunity also fades over time. Annual vaccination ensures healthcare workers (HCWs) have up-to-date protection each flu season. The CDC’s expert panel, “ACIP,” recommends that all healthcare personnel get a flu vaccine annually to reduce illness and death in workers and patients. In other words, it’s not just about you; it’s about the people you care for.
Healthcare workers are more likely to be exposed to the flu than most people (after all, hospitals are magnets for viruses). If a nurse or doctor catches the flu, they might spread it to high-risk patients before even realizing they’re sick. Tragically, flu can be deadly for vulnerable groups like the elderly, chronically ill, or immunocompromised patients. By vaccinating staff, hospitals create a protective shield around patients. One medical ethicist put it bluntly: Vaccinating healthcare staff against flu should be considered standard patient care, and not doing so is essentially doing harm. “Do no harm” is healthcare’s core ethic – and spreading flu to patients is definitely harm.
Why every year? The influenza virus is a shape-shifter. The circulating strains differ each year, and the vaccine is updated to match them. Plus, immunity from the shot wanes within months. So last year’s shot won’t reliably guard you a year later. A fresh flu vaccine each year is the best way to maintain immunity throughout the flu season, which generally lasts from fall through early spring.
Key reasons annual flu shots are a must for HCWs: (in case you need talking points):
· Protecting Patients: You’re around sick, fragile people every day. A flu shot helps ensure you don’t become a flu vector carrying the virus to a patient’s bedside.
· Protecting Yourself: Healthcare workers who get vaccinated are less likely to catch influenza. No one enjoys coughing through rounds or using up PTO in bed with a fever.
· Workforce Readiness: Vaccinated staff mean fewer call-outs and a more resilient team during peak flu season. Hospitals need all hands on deck when illness spikes.
· Community Health: By staying healthy, you’re not bringing the flu home to your family or spreading it in the community. It’s a ripple effect of protection.
· Because It’s Policy: If your hospital mandates it, it’s required! But that policy exists for all the reasons above (as we’ll see, it’s backed by evidence).
Flu Vaccine Effectiveness: By the Numbers
Let’s address the big question: How well do these flu shots work? We’ve all heard someone say, “I got the shot and still got sick.” Indeed, the flu vaccine isn’t 100% foolproof, but influenza is a tricky virus, and it significantly reduces your risk of getting ill. Recent CDC data show that the vaccine can reduce the risk of flu illness by approximately 40–60% in the overall population when it is well-matched to circulating strains. Flip that around: even in a not-so-great year, your odds of getting sick are much lower with the shot than without.
Some studies have found even higher effectiveness among healthcare workers. In one randomized trial, the flu vaccine was remarkably ~88% effective against influenza A and 89% against influenza B in HCWs that season. (That was measured by who developed antibodies and confirmed infections – pretty robust results!). Not every year will hit those numbers, of course, effectiveness varies, but even moderate protection is better than none. Importantly, even if a vaccinated person does get the flu, their illness is often milder and shorter, and they’re less likely to develop serious complications.
There’s also indirect effectiveness: when more staff are immune, flu spreads less within the hospital. It’s a bit of herd immunity in the workplace. Fewer carriers mean fewer chances for an outbreak to spark. That’s where the real payoff comes in a healthcare setting, reducing the number of viruses floating around the ICU, oncology ward, or nursing home.
Research backs this up. A meta-analysis found that vaccinating healthcare personnel significantly reduced infections and absenteeism among staff, even enough to outweigh the costs of the vaccination program (fewer sick days saved money in the end). Consider this: if your hospital vaccinates, say, 1,000 employees, preventing even a fraction from falling ill can save hundreds of lost workdays. And for those who do catch flu despite the shot, studies suggest they may have lower odds of severe outcomes like hospitalization or pneumonia compared to unvaccinated folks.
It’s worth noting that effectiveness can fluctuate. Some years, the flu strains mutate unexpectedly, and the vaccine match is suboptimal so that protection might be on the lower end. Other years, it’s spot on. But even in “off” years, the vaccine still provides some protection and can lessen severity. As an HR colleague, I often tell skeptical staff: “Sure, you might still get the flu, but I’ll bet you’d rather have a milder case than the full-force version!” Most nod in agreement.
To summarize the data in plain terms: flu shots are far from perfect, but they’re our best defence. They consistently lower a person’s chance of getting sick and help create a safer bubble in healthcare settings. When you multiply that effect across an entire hospital staff, the impact on reducing overall infections is huge. And that leads us to the real bottom line – protecting our patients.
Vaccination Protects Patients: Better Outcomes and Safety
One of the strongest arguments for mandating flu shots in hospitals is patient safety. We’ve hinted at it already; by keeping healthcare workers flu-free, we indirectly shield those under our care. The evidence gets pretty inspiring here. Several studies have shown that when healthcare personnel are vaccinated, their patients fare better.
For example, a comprehensive review of clinical trials found that patient mortality dropped noticeably in units where staff were encouraged or required to get flu shots. In fact, across multiple long-term care trials, all-cause patient deaths were about 29% lower when healthcare workers were vaccinated vs. not (risk ratio 0.71). That’s a striking statistic – nearly one-third fewer deaths, presumably because vulnerable patients weren’t catching flu from caregivers. The same analysis also showed 42% fewer cases of influenza-like illness in patients when staff were vaccinated (risk ratio 0.58). Fewer fevers, coughs, and severe flus among patients – simply by immunizing the people who care for them. The authors concluded, “HCP influenza vaccination can enhance patient safety.”
Another study in a cancer hospital demonstrated a similar benefit: when the hospital increased staff vaccination rates, nosocomial (hospital-acquired) influenza infections in patients significantly declined. In that case, they observed a statistically significant decrease in patient flu cases (P = 0.045) once more employees began receiving vaccinations. Patients in oncology or ICU can be highly susceptible to flu complications, so preventing just one transmission could save a life.
Real-world hospital experiences echo these findings. Remember our story of the mini-outbreak at the start? Contrast that with what happened at the Children’s Hospital of Philadelphia (CHOP) after they introduced a strict vaccination policy. Over the past decade, CHOP has required annual flu shots for all staff, resulting in employee vaccination rates increasing from 91% to 99.3%. As a result, the rate of healthcare-associated flu cases in patients plummeted from a median of 16.8 cases per season down to 5.2 cases, a ~69% reduction. That’s a tangible drop in sick kids. Fewer sick staff = fewer sick patients. In infection control, that’s the dream outcome.
Even beyond flu-specific outcomes, maintaining staff health has a ripple effect on patient care quality. Fewer staff members out sick means units are less understaffed during peak illness weeks, allowing patients to receive proper care. Staff not battling illness are at their best, alert, energetic, and focused on patients. It all ties back into quality and safety.
From an HR standpoint, I’ve seen how emphasizing patient safety resonates with hospital employees. Healthcare folks are altruistic by nature; they want to protect patients. When you share stats like “getting our staff vaccinated could cut our patients’ flu risk nearly in half” or stories like the CHOP's success, it clicks. It turns a “mandatory HR task” into a mission everyone can get behind.
Simply put, flu vaccination isn’t just about individual wellness; it’s a form of infection control. It’s akin to hand hygiene or wearing PPE: another practice that keeps patients safe from something we could inadvertently transmit. Hospitals with high staff vaccination rates have observed lower patient mortality, fewer outbreaks on wards, and healthier patient populations during flu season. For HR and hospital leadership, that’s powerful motivation to aim for near-100% compliance. Lives may be at stake, and a shot in the arm can tilt the odds in everyone’s favour.
Mandates Work: How Requiring the Flu Shot Raises Compliance
So if flu vaccines are so beneficial, why don’t all healthcare workers just roll up their sleeves? The reality is, without a nudge or requirement, many won’t. Voluntary vaccination rates among healthcare staff can be subpar, often falling short of the ideal. That’s where mandates come in, and the evidence is crystal clear: making the flu shot a requirement (with appropriate exemptions) sends vaccination rates through the roof.
Take national data from the U.S. 2022–2023 season: among healthcare personnel whose employers required a flu vaccine, about 95% got vaccinated. In contrast, coverage was only ~77% if the employer just “recommended” it, and a dismal ~55% if no recommendation or requirement was in place. In other words, almost all healthcare workers will get the shot when it’s mandated, whereas nearly half skip it if it’s optional. That difference is huge. It can be the gap between protecting your staff versus leaving patients at risk.
The graph below (from CDC’s flu vaccine surveillance) illustrates this point. It shows healthcare worker flu vaccination rates by work setting over the past decade. Hospitals (which increasingly require vaccination) are the top line, with consistently high rates, while long-term care facilities (often with looser policies) lag behind. The trend is clear; stronger policies equal higher uptake.
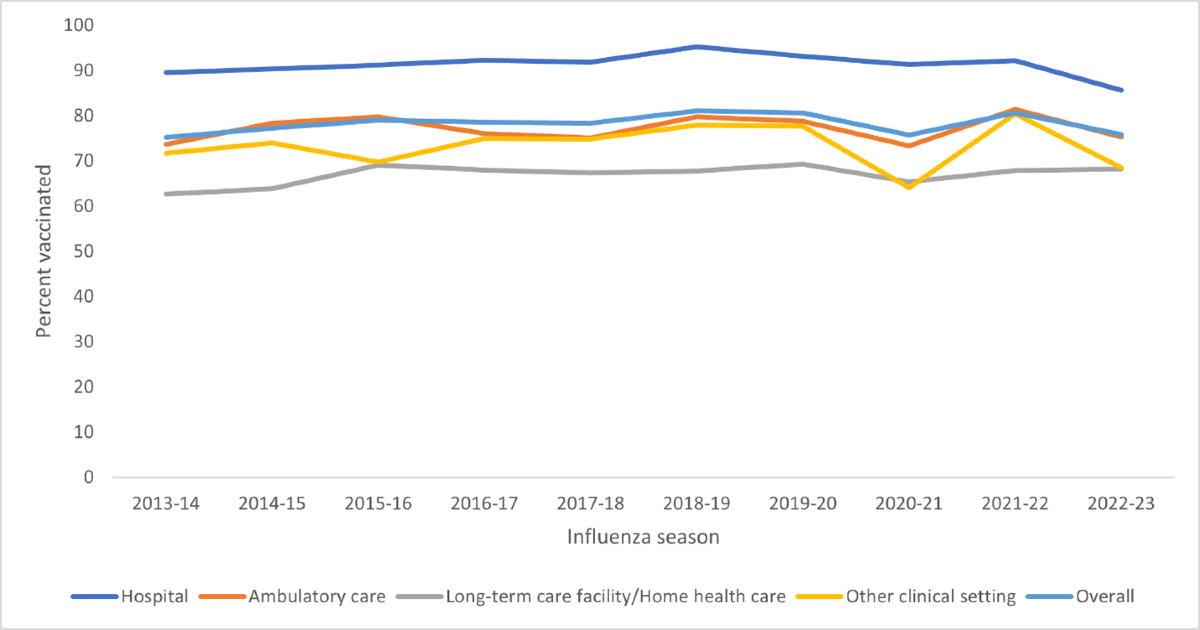
Figure: Percentage of healthcare personnel vaccinated against flu by work setting (2013–2023). Hospital staff (blue line) maintain the highest vaccination rates, whereas long-term care and home health workers (orange line) have lower rates, reflecting differences in vaccination requirements.
In recent years, hospital mandates have become the norm rather than the exception. A 2024 study found that 74% of U.S. general hospitals now require staff to get an annual flu shot (or formally opt out with an exemption). The rate among VA hospitals (serving veterans) was even higher at 96%, thanks to a new VA directive. Compare that to 2013, when less than half of hospitals had any flu shot requirement. We’ve seen a significant shift in a decade – driven by the recognition that mandates effectively protect patients and staff. Many hospitals also implement “soft” mandates, such as declination forms or requiring unvaccinated staff to wear masks. Even those measures can boost rates somewhat, but nothing beats a firm requirement.
What kind of results do hospitals see with mandates? Let’s look at a couple of success stories:
· Virginia Mason Medical Center (Seattle): one of the pioneers of mandatory flu vaccination. After implementing their requirement (with the alternative of wearing a mask for those exempt), they hit coverage above 98% and kept it there for 5+ years straight. Exemptions were tiny (<0.7%), and virtually no employees quit over it (<0.2%). Essentially, everyone got on board, and the policy became routine.
· Children’s Hospital of Philadelphia (CHOP): as mentioned earlier, CHOP went from 91% compliance to 99.3% of employees vaccinated after making flu shots mandatory, sustained over a decade. The number of exemption requests dropped dramatically too (from 2.5% of staff to just 0.3%). Importantly, over those years, only five employees had to be terminated for refusing to be vaccinated. Out of thousands of staff, only five ultimately failed to comply – an incredibly low fallout rate, indicating that mandates with education can bring nearly everyone on board.
Other hospitals report similar outcomes: when a flu shot becomes a condition of employment, compliance typically exceeds 95% (often even 98–99%). Compared to the ~60–70% coverage many hospitals had with voluntary programs in the past. Mandates usually increase vaccination rates by an additional 20–30 percentage points or more, which is massive.
And higher vaccination rates aren’t the only benefit; hospitals also see fewer flu outbreaks and improved metrics after instituting mandates. CHOP’s ~70% reduction in patient flu cases was one example. Another hospital reported a decrease in staff sick days (although not always statistically significant in every study) and an improvement in continuity of care during flu season. It’s challenging to accurately measure the full extent of avoided illness and complications, which are largely attributed to widespread vaccination. Still, infection prevention experts will tell you those silent victories are the goal.
From an HR perspective, having a mandate simplifies the expectation: it’s clear that everyone (barring exemptions) needs a shot. That clarity can make compliance more straightforward to manage than a voluntary program, because you’re not perpetually coaxing the maybe/maybe-not folks – it becomes a standard checklist item like an annual TB test or license renewal. In many hospitals, flu vaccination compliance is now treated as part of employee credentialing each year, often due by a specific date (e.g. “get your shot by November 1st or you can’t work”).
It’s worth noting that mandates should always include provisions for valid medical or religious exemptions, as nearly all do. But even with some exemptions, you can still hit very high coverage. Hospitals commonly see only 1–2% of staff exempt for medical reasons (such as severe allergies) and a small fraction with religious exemptions. The overall result is that well over 95% of personnel are immunized, which is sufficient to drastically reduce transmission.
In short, mandates work. They achieve what education, free coffee gift cards, and “please get your flu shot” emails alone often could not. When it’s required, most people comply, and as we’ve established, that leads to safer hospitals. Next, we’ll discuss getting everyone on board and handling the bumps in the road that can come with implementing such a policy.
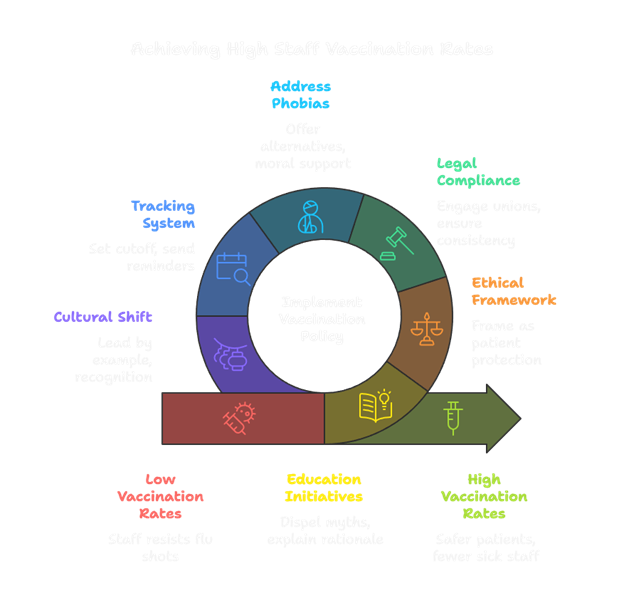
Overcoming Challenges: How Hospitals Address Concerns and Resistance
Mandating a medical intervention, even a routine one like a flu shot, isn’t without challenges. HR and management often have to navigate various concerns from staff when rolling out or enforcing an annual flu vaccination policy. Let’s talk about some common challenges and how many hospitals have overcome them:
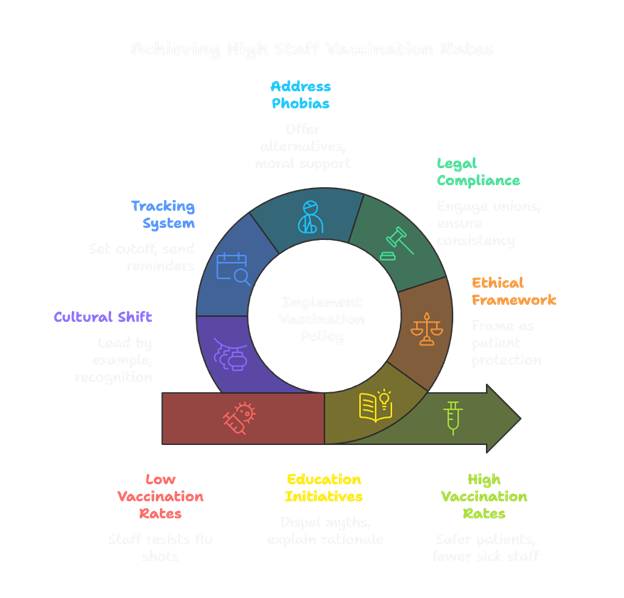
1. Staff Resistance and Personal Beliefs: There will always be a subset of employees hesitant about vaccines. Reasons vary; some have misinformation (“the flu shot gave me the flu once”), others doubt its effectiveness, and some simply dislike being told what to do. To address this, education is key. Hospitals have found success holding info sessions, Q&As, or one-on-one counselling to dispel myths and explain the why. For example, explaining that the injected flu vaccine is an inactivated virus (it cannot cause flu), and that soreness or mild fever afterward is just the immune system kicking in, not an infection. Sharing facts like “studies show the vaccine cuts your risk of getting flu by about half” or “unvaccinated healthcare workers can indeed spread flu to patients” helps ground the mandate in patient safety. Many resistant staff come around when they understand the impact and see hospital leadership and peers all getting the shot too.
2. Ethical or Autonomy Concerns: Some argue that requiring a vaccine infringes on personal autonomy or is “unethical.” It’s a delicate balance; yes, we value personal choice, but the duty to protect patients can outweigh individual preferences in healthcare. Ethically, it’s often framed this way: patients can’t defend themselves (they can’t choose their nurse’s vaccine status), so it’s on us, as healthcare providers, to do no harm. The overwhelming stance of professional bodies is that patient safety justifies these requirements. Many hospitals present it as a professional obligation, akin to wearing gloves to prevent harm. That said, providing opt-out paths for those with sincere religious objections or true medical contraindications is essential. Having a clear, fair exemption policy (with documentation for medical exemptions, and a process for reviewing religious ones) shows respect for individual circumstances while still holding the line on overall safety. Interestingly, one survey noted that about 40% of healthcare providers initially viewed mandatory vaccination as unethical in theory. Still, with proper communication about the rationale, most organizations have gained acceptance that it’s ultimately about protecting others.
3. Labour and Legal Hurdles: Hospitals sometimes worry about pushback from employee unions or even legal challenges. However, in practice, flu shot mandates have held up well legally, especially when they allow medical/religious exemptions. Early engagement with labour representatives, if applicable, can help, emphasizing that this is about workplace safety (similar to required Hepatitis B vaccination or MMR for hospital staff, which are long-standing). It also helps to implement the policy with plenty of notice and input. Some hospitals phase it in by strongly encouraging and offering free on-site vaccination, then making it mandatory the following year once resources are in place. As long as the policy is applied consistently and exemptions are handled appropriately, the legal risk is low. In fact, the Equal Employment Opportunity Commission (EEOC) recognizes that hospitals can mandate vaccines for safety, as long as accommodations are made for valid exemptions. Solid HR policies and documentation are your friend here – have employees sign an acknowledgement of the requirement, track who’s vaccinated, who’s exempt, and ensure non-compliant staff don’t slip through.
4. “Needle Phobia” or Fear of Side Effects: Some people just hate needles or worry they’ll feel unwell after the shot. For these, convenience and compassion help. Make vaccination clinics highly accessible by setting up stations in the cafeteria, units, and employee health facilities, and consider offering alternatives, such as the intranasal vaccine, if appropriate (although it’s limited to certain ages/conditions). Offer shots during all shifts so the night staff can easily get them. Emphasize that the most common side effect is a sore arm and possibly feeling a bit achy for a day, which is far milder than an actual flu illness. Peers can encourage each other (“I got mine, it wasn’t bad at all!”). I’ve seen departments do friendly challenges or competitions, which add a fun element. For needle-phobes, having skilled, gentle nurse vaccinators on hand who can talk them through it makes a difference – a little moral support goes a long way.
5. Tracking and Enforcement: A practical challenge is ensuring everyone gets it done by the deadline, especially in large hospitals. Chasing down procrastinators can be tedious for HR or managers (we’ll discuss a solution for that in the next section!). Many hospitals handle this by setting a firm cutoff date before peak flu season and sending regular reminders. Those who haven’t complied may receive escalating communications: first an email, then a personal call, and finally a notice that they will be removed from the schedule if not compliant by a specified date. It rarely comes to that because nearly everyone falls in line when the seriousness is clear. Some places use the approach “Vaccinate, or sign an official declination (for those few who refuse), and you must wear a mask near patients for the whole flu season.” While not as ideal as vaccination, that mask policy often serves as a deterrent; most folks would rather get a quick shot than wear a stuffy mask for months (though after COVID, masks are less of a deterrent than they used to be!). Still, it’s a measure that can allow a tiny number of holdouts to work with reduced risk to patients. Over time, however, many hospitals have adopted true mandates without a mask opt-out, because they found that almost everyone complies.
6. Cultural Change: At the end of the day, getting to near-100% vaccination in a hospital is a cultural shift. Early on, there may be grumbling, “why is this mandatory all of a sudden?”, especially among folks who never got a flu shot. Leadership and management need to set the tone. Lead by example: when the CEO, CNO, and physician chiefs are first in line for the vaccine, it sends a message. Recognize and thank staff for doing their part. Some organizations celebrate hitting their 98% target with a pizza party or simple shout-outs. It’s about making flu vaccination part of “how we care for patients here.” In a couple of years, most hospitals will find that it has become just an ordinary routine, not a major struggle. New hires are informed from day one that flu shots are expected. Momentum builds, and resistance tends to wane as new norms take hold.
By tackling these challenges with empathy, information, and a firm focus on patient safety, hospitals have achieved extraordinarily high vaccination rates among their staff. Many who initially objected often come around once they understand why it’s important, or simply because it’s required and everyone around them is doing it. In the end, pride can replace resentment when people see that the policy genuinely leads to fewer sick coworkers and safer patients. HR plays a crucial role in this change management, striking a balance between enforcement, education, and support. Fortunately, modern tools can make compliance logistics significantly easier, which brings us to…
The HR Toolkit: Using Digital Tracking to Ensure Compliance (and Keep Your Sanity)
If you’re in HR or occupational health, you know that tracking hundreds or thousands of employees’ flu vaccination status can be an administrative nightmare. In the “old days,” this might have involved Excel spreadsheets, paper consent forms, endless email reminders, and Post-it notes all over your desk. It’s enough to give even the most organized HR pro a headache. Enter digital tracking tools, such as Expiration Reminder, which are game changers for managing vaccination compliance with far less effort.
So, what can an automated tracking system do for you? In a nutshell: monitor who’s gotten their shot, who hasn’t, send automatic reminders, log exemptions, and generate reports – all without manual data crunching. Let’s break down the benefits:
- Automated Reminders: Instead of personally emailing John in radiology for the 4th time about his flu shot, a system like Expiration Reminder will send customizable email or text reminders to employees who haven’t provided vaccination proof yet. For example, a month before the deadline, everyone due could get a friendly nudge. As the deadline approaches, the tone can escalate – “Action Required: Flu vaccination due by Oct 31.” These notifications can also loop in supervisors. In one study, a hospital that implemented automated reminders for workers and managers achieved over 98% compliance without requiring nearly as much manual follow-up.
- Real-Time Tracking Dashboard: A good platform provides a dashboard that allows you to view, at a glance, your overall compliance rate and identify those who are pending. Expiration Reminder, for instance, will list employees and show whether their vaccination status is current or expired (or due soon). It’s colour-coded and intuitive – no special IT skills needed. You can filter by department, role, etc., which is handy if you need to prod a lagging specific unit. This means no more sorting spreadsheets for hours; you log in and immediately know where things stand.
- Exemption Management: Handling exemptions can be a sensitive and complex process. A digital tool can track who has submitted a medical note or religious exemption request, whether it has been approved, and even set reminders for any follow-up (some medical exemptions may need to be renewed each year, for example). Instead of sticky notes about “Dr. Smith – egg allergy, needs exemption,” the system keeps a secure record. Ensure that those individuals are noted as exempt (so they don’t continue to receive pestering reminders), and have documentation ready in case anyone asks. It also helps in reporting – e.g., you can quickly tally “we have 12 medical exemptions and five religious exemptions this year” if leadership wants to know.
- Policy Enforcement & Escalation: Digital platforms can often integrate with HR systems to enforce policies. Some hospitals configure their systems so that if an employee is non-compliant by the deadline, an alert is sent to their manager and potentially even to scheduling or badge access systems. I’ve seen setups where an unvaccinated employee’s ID badge gets deactivated (temporarily) until they comply or get an exemption. While that sounds harsh, it’s an effective last-resort mechanism and underscores the seriousness. Short of that, even having the data to know exactly who to call in for a stern talk is valuable. With an automated tracker, the list of stragglers is always up to date.
- Reduced Administrative Burden: This is perhaps the most significant benefit, resulting in significantly less paperwork and stress for HR/employee health teams. One study published in the Infection Control & Hospital Epidemiology journal showed that implementing an electronic tracking and reminder system cut the time occupational health staff spent on the vaccination program by 56% and accounted for 98% of the compliance achieved, with only minimal manual follow-up needed. Imagine cutting over half of the overtime and hassle out of flu season! The automation shifted responsibility to individual employees and their supervisors to complete the task, rather than having HR oversee the process. In practical terms, HR can focus more on education and other responsibilities instead of filling out forms.
- Audit-Ready Reports: Healthcare organizations often need to report vaccination rates to various bodies (for instance, the Joint Commission or state health departments might ask, and in the U.S., acute care hospitals report flu vaccine coverage data to NHSN/CDC annually). Expiration Reminder and similar tools can generate reports with a single click, displaying the overall compliance percentage, lists of non-compliant staff, and more. These are audit-ready, meaning if someone asks “prove that all your staff met the requirement,” you can produce documentation quickly. It’s also useful for internal quality improvement – you can easily compare year-to-year statistics.
- Self-Service for Employees: Some systems allow employees to log in and upload their proof of vaccination or update their status. For example, if someone got vaccinated at their local pharmacy instead of the hospital clinic, they can snap a photo of the documentation and upload it. This self-service approach saves HR the step of manually entering data. Expiration Reminder even has a feature that allows you to send a secure link to staff, enabling them to update their records without requiring a full account login. The easier you make it for employees to report their vaccination status, the higher the compliance you’ll achieve with less chasing.
To illustrate, the University of California Irvine Health adopted an automated tracking system for its mandatory flu shots. It would email anyone who hadn’t confirmed their vaccination, and managers could see their team’s status on an intranet site. The result? Of ~7,000 staff, over 98% were compliant via the automated system alone, only 130 people needed a personal warning, and just five had to be taken off the schedule for non-compliance. They also saved a ton of staff hours. One of the study authors, Dr. Susan Huang, noted that automation let them enforce the policy “without excessive diversion of skilled labor and resources” – freeing up their infection prevention team to focus on other priorities.
Expiration Reminder, as a tool, fits precisely into this picture. It’s designed to track expiration dates and compliance for certifications– an annual vaccine is essentially an expiring certification each year. You set the flu shot with a due date, assign it to all employees, and let the software handle the routine follow-ups. It will ping people ahead of time, alert you to who is overdue, and keep records of everything. HR can then spend time on the human side (education, answering questions, coordinating vaccine clinics) rather than on data management.
From my experience, implementing a digital tracker is a relief. One HR colleague joked that flu season used to mean “time to enter dread mode,” but now the system does the heavy lifting, and she just monitors a dashboard with a coffee in hand. For anyone concerned about complexity, these systems are generally user-friendly and cloud-based. No messy installation; often it’s a simple web interface. Data security is top-notch, too (important for health info). In short, technology has our back.
The bottom line for HR is that if your hospital mandates (or is moving toward mandating) flu vaccines, invest in a good tracking solution. It ensures no one slips through the cracks, keeps everything organized, and significantly reduces administrative workload. Tools like Expiration Reminder transform what could be a chaotic spreadsheet process into a streamlined one with real-time compliance visibility and automatic follow-ups. It’s like having a personal assistant dedicated to vaccination tracking, one that never forgets a deadline or gets tired of sending reminders!
Conclusion: Protecting Lives, Easing Work – A Win-Win
Ultimately, the annual influenza vaccination campaign in healthcare isn’t just a bureaucratic hoop to jump through; it’s a cornerstone of patient safety and workforce well-being. As we’ve discussed, the rationale is clear: a vaccinated healthcare team means less flu spreading around our hospitals. That translates to fewer vulnerable patients getting sick (or dying) from a preventable exposure, and it keeps our doctors, nurses, and staff on their feet to care for those who need them.
We’ve seen the data: flu shots substantially reduce the risk of infection, and when nearly everyone in a hospital is vaccinated, patient outcomes improve, ranging from lower mortality rates to fewer hospital-acquired flu cases. We’ve also seen that mandates make a huge difference in achieving those high vaccination rates, with many hospitals now reaching over 95% compliance and making annual flu shots as routine as washing hands. The success stories show it’s possible to get an entire workforce on board, and the “stick” of a mandate often comes with the “carrot” of a safer workplace and healthier patients that staff can take pride in.
There are challenges, but as we explored, they can be managed with thoughtful strategies – from education campaigns to listening to concerns and offering convenient access. Many hospitals have gone through the initial bumps and now have a culture where getting your flu shot each fall is “what we do because we care about our patients and each other.” As HR professionals and healthcare leaders, fostering that culture is one of the best things we can do.
Thankfully, we don’t have to do it the hard way. Modern HR tools like Expiration Reminder alleviate the administrative burden, letting us ensure compliance without losing our sanity. Automated tracking and reminders mean no one forgets, and you’ll know exactly who needs that extra nudge. It transforms a daunting annual project into a smooth, repeatable process.
To wrap up on a conversational note: Getting that flu shot is a small act each of us in healthcare does once a year, but its impact echoes through the entire community. It’s a few seconds of discomfort for months of protection, a trade-off we, HR folks, must encourage and sometimes enforce, for the greater good. When you see a high-risk patient make it through winter without catching the flu, or you notice your staff had far fewer sick call-outs, you realize those jabs in the arm prevented a lot of suffering.
So, as flu season looms, let’s continue championing vaccination in our hospitals. It’s one of the easiest ways to save lives and show we care. With strong policies, supportive education, and the right tracking tools, we can achieve near-universal flu vaccination among healthcare workers year after year. That’s a legacy of safety and trust worth striving for, one flu shot at a time.
Stay healthy, keep those sleeves rolled up, and here’s to a flu-free workplace! 👩⚕️💉👨⚕️


%20(34).png)

.webp)
.webp)