Table of Contents
Best Practices for Tracking Employee Certifications in Healthcare
The compliance officer at a 250-bed hospital in Ohio had just received notification: The Joint Commission surveyors would arrive in two weeks. She pulled up her staff certification tracking spreadsheet—the one she'd maintained for three years—and felt her heart sink.
Scrolling through hundreds of rows, she spotted it: an RN working in the ICU whose license had expired 12 days ago. Then another—a respiratory therapist with a lapsed CPR certification. As she dug deeper, she found seven more credentials that had slipped through unnoticed.
The panic wasn't just about the upcoming survey. Those expired certifications represented genuine patient safety risks, potential regulatory violations, and a compliance nightmare that could cost the hospital its accreditation.
Sound familiar? If you're managing employee certifications in healthcare, this scenario probably hits close to home. The stakes are high, the volume is overwhelming, and manual tracking methods simply can't keep up with the complexity.
In this guide, we'll walk through healthcare best practices for tracking employee certifications that eliminate these risks, reduce administrative burden, and keep your organization audit-ready without the daily stress.
Why Healthcare Certification Tracking Demands Better Systems
Healthcare operates under some of the strictest regulatory oversight in any industry. State licensing boards, The Joint Commission, CMS, OSHA, and specialty accreditors don't just recommend that clinical staff maintain current credentials—they mandate it.
When certification tracking fails, the consequences are severe.
According to the American Hospital Association's 2025 healthcare forecast, workforce challenges remain the top strategic priority for health system executives. When you're already stretched thin, losing a staff member to a preventable credential lapse makes a bad situation exponentially worse.
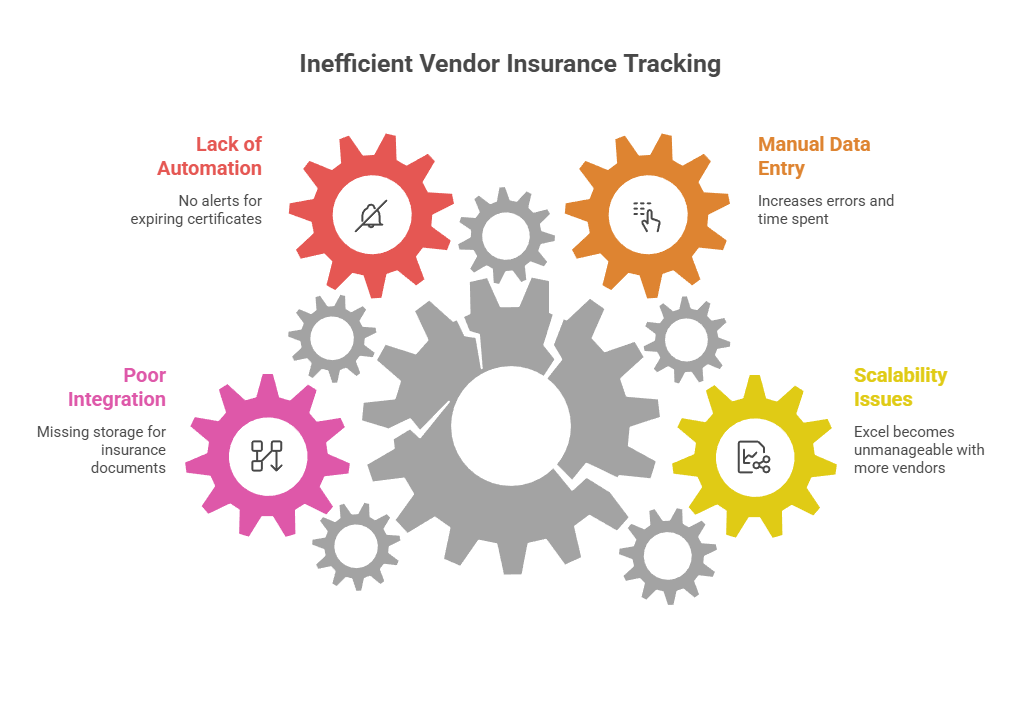
The Critical Gap: Where Traditional Tracking Methods Fail
Before diving into best practices, let's acknowledge where most healthcare organizations struggle with certification management.
Spreadsheet Dependency Creates Systemic Risk
Excel spreadsheets remain the most common tracking tool—and the single biggest point of failure. One hospital HR director described her experience: "I inherited a massive Excel file with separate tabs for every department and credential type. Half the expiration dates were formatted as text instead of dates, conditional formatting was broken, and I had no confidence the information was even current. I spent my entire first month just trying to clean it up—and I still found gaps during our survey."
Decentralized Record-Keeping Guarantees Gaps
In many healthcare organizations, responsibility for credential tracking gets fragmented across multiple departments.
When records live in silos, no single person has a complete compliance picture. Critical items fall through the cracks between departments. During regulatory surveys, assembling everything becomes a frantic, multi-day scavenger hunt that pulls people away from patient care.
Reactive Management vs. Proactive Prevention
Most organizations discover expired credentials rather than preventing expirations. Without automated early warning systems—at 90 days, 60 days, 30 days, and 15 days before expiration—staff don't have adequate time to schedule courses, complete required hours, or submit renewal applications.
Last-minute renewal attempts create unnecessary stress, increase the likelihood of lapses, and often result in expensive expedited processing fees or temporary credentialing gaps.
Inadequate Documentation of Proof
Tracking expiration dates alone isn't sufficient for regulatory compliance. During surveys, auditors require copies of actual certificates, licenses, course completion records, and renewal documentation.
If you're tracking dates in a spreadsheet but storing supporting documents in physical file cabinets, scattered email attachments, or shared drives with inconsistent naming conventions, you'll fail the audit test—even if technically no credentials have expired.
Best Practice #1: Centralize All Certification Data in a Single System
The foundation of effective healthcare certification tracking is establishing a single source of truth where every employee credential lives and is managed.
Centralization doesn't mean one person does all the work. It means all stakeholders use one system where updates are visible in real time. For example: a nurse uploads her renewed BLS card through a self-service portal, her manager receives an automatic notification and approves it, HR sees the update immediately, and compliance can pull current reports whenever needed.
Implementation action: Conduct an audit identifying where certification data currently exists in your organization—every spreadsheet, database, filing cabinet, and software system. Document the gaps and inconsistencies, then commit to migrating everything into a unified platform.
Best Practice #2: Implement Multi-Stage Automated Reminder Workflows
Manual reminder systems—calendar alerts, sticky notes, or monthly spreadsheet reviews—don't scale reliably across dozens or hundreds of staff members. Automation ensures nothing slips through organizational cracks.
Establish a system that automatically sends progressive reminder sequences:
Reminders should utilize multiple communication channels—email for detailed instructions and documentation, SMS for urgent time-sensitive alerts. Each notification should include clear guidance: what needs renewal, where to find approved training providers or renewal forms, submission deadlines, and who to contact with questions.
Managers also need aggregated views rather than individual alerts. A weekly or monthly summary showing all upcoming expirations within their department allows proactive discussion during one-on-ones and staff meetings.
Implementation action: Map your ideal reminder timeline for each credential type (some may need longer lead times than others). Define notification recipients at each stage. Select or configure a platform capable of executing these workflows automatically without manual intervention, and eliminate missed renewals today.
Best Practice #3: Assign Clear Ownership and Accountability at Every Level
Even the most sophisticated tracking system fails without clear accountability structures.
Define explicit roles for:
Employee responsibilities
Manager responsibilities
HR/Compliance responsibilities
Make expectations explicit in job descriptions, new employee orientation, annual competency training, and credentialing policies. For example: "All clinical staff must maintain current BLS certification as a condition of employment and clinical practice. You will receive automated renewal reminders via email and SMS at 90, 60, 30, and 15 days before expiration. Completion of renewal and submission of proof documentation is required no later than 7 days before current certification expires."
Track accountability through your system's audit log functionality. If a license lapses, documentation should show whether automated reminders were sent, whether the employee acknowledged them, what follow-up occurred, and what barriers were identified.
Implementation action: Draft or update your credential maintenance policy document. Include specific timelines, individual responsibilities at each organizational level, escalation procedures, and consequences for non-compliance. Train all stakeholders on their roles.
Best Practice #4: Maintain Continuously Audit-Ready Documentation
Regulatory surveyors and auditors require proof, not promises.
Your system must enable rapid production of:
Individual credential files: Complete documentation packets for any employee showing all required licenses, certifications, and supporting proof documents with clear validity dates
Compliance reports by credential type: Instant answers to questions like "Show me all BLS certifications expiring in the next 60 days" or "Prove that every RN currently working has a valid state license"
Historical compliance records: Demonstration of continuous compliance over time, not just current snapshot status
Complete audit trails: Documentation showing who verified credentials, when documents were uploaded, who approved them, and any modifications made to records
Store high-quality digital copies of all documentation—scanned licenses, downloaded course completion certificates, photographed certification cards. Implement consistent file naming conventions (e.g., "LastName_FirstName_CredentialType_ExpirationDate.pdf") and link documents directly to the associated record in your tracking platform.
During a regulatory survey, you should be capable of generating a complete compliance report and exporting all supporting files within 30 minutes, not 30 hours.
According to CMS Conditions of Participation guidelines, healthcare organizations must verify and document credentials before allowing clinical staff to provide patient care, and maintain evidence of current licensure, certification, and training at all times.
Implementation action: Conduct a mock audit exercise. Randomly select five employees and attempt to produce complete, compliant credential files for each within 30 minutes. Document gaps, missing proof documents, and process inefficiencies. Use findings to improve your documentation workflow.
Best Practice #5: Leverage Purpose-Built Certification Tracking Technology
Healthcare best practices increasingly rely on specialized software designed specifically for compliance and expiration management rather than generic tools repurposed for tracking.
For example, Expiration Reminder centralizes all types of credentials—not just employee certifications but also facility permits, vendor insurance certificates, equipment inspections, and contract renewals—into one secure, compliant platform. Healthcare organizations use it to track everything from individual clinical licenses to departmental accreditations, set up custom reminder sequences specific to each credential type, attach unlimited supporting documents, and generate audit-ready reports instantly.
Unlike generic project management tools, basic spreadsheets, or calendar apps, a dedicated expiration tracking system is built specifically for compliance workflows. It proactively prevents lapses through automated reminders via email and SMS, maintains complete audit trails of every credential update, stores supporting documentation securely, and scales effortlessly as your workforce grows.
The platform is HIPAA compliant, SOC 2 certified, and meets the security standards required for healthcare organizations handling sensitive employee information.
Implementation action: Evaluate your current technology stack. If you're relying primarily on spreadsheets, email reminders, or manual processes, explore dedicated certification management platforms. Request demonstrations from 2-3 vendors. Compare features, security compliance, integration capabilities, ease of use, and total cost of ownership.
Best Practice #6: Standardize Processes and Train All Stakeholders
Technology only delivers value when people use it correctly and consistently. Develop standard operating procedures (SOPs) documenting and provide comprehensive training for all user groups.
New employee orientation: How to access the credential portal, view personal expirations, upload renewal documentation, and respond to reminders
Manager training: How to run departmental reports, interpret compliance dashboards, address non-compliant staff, and support timely renewals
HR/compliance training: System administration, report generation, audit preparation, data integrity verification, and advanced features
Annual refreshers: Policy updates, new credential requirements, system enhancements, and lessons learned from recent surveys
Document all SOPs in accessible locations: Your organization's intranet, policy manual, or learning management system—and keep them current as processes evolve.
Implementation action: Create a one-page quick-reference guide for employees titled "How to Keep Your Certifications Current and Upload Proof." Include screenshots, key deadlines, acceptable documentation formats, and FAQs. Distribute during onboarding and post in break rooms, nursing stations, and your employee portal.
Best Practice #7: Monitor Compliance Metrics and Drive Continuous Improvement
What gets measured gets managed. Establish key performance indicators (KPIs) to ensure your certification management program stays on track.
Critical compliance metrics: Review these metrics at least monthly with senior leadership and department heads. Celebrate improvements and address problem areas systematically. If one department consistently has late renewals, investigate whether it indicates inadequate staffing for course attendance, manager inattention, budget constraints, or other correctable issues.
Visual dashboards displaying compliance status by department, role, and credential type make trends immediately apparent and support data-driven decision-making.
Implementation action: Identify three to five KPIs most critical to your organization's compliance goals. Configure automated monthly reports or real-time dashboards. Schedule standing monthly review meetings with stakeholders to assess trends and implement corrective actions.
Best Practice #8: Plan Proactively for Workforce Transitions
Healthcare workforce turnover and role changes can disrupt credential tracking. Build transition management into standard processes for:
Departing employees
New manager transitions
Role changes and promotions
Implementation action: Add credential tracking items to your organization's standardized onboarding, offboarding, and internal transfer checklists. Ensure HR or compliance receives automatic notifications for every hire, termination, and role change.
Best Practice #9: Integrate Certification Tracking with Broader Compliance Programs
Employee credentials are one component of your organization's total compliance landscape.
Your tracking approach should integrate with:
Medical staff credentialing and privileging: Physician and advanced practice provider credential verification, primary source verification, ongoing professional practice evaluation, and privilege delineation.
Competency assessment programs: Skills validation beyond credential possession, including demonstration of clinical competencies, equipment operation proficiency, and procedure-specific training.
Infection prevention and occupational health: Immunization status, declination documentation, TB screening, bloodborne pathogen exposure protocols, and respiratory fit testing.
Environment of care and safety: Facility permits and licenses, equipment maintenance records, safety inspection certifications, and hazardous materials handling credentials.
Quality and performance improvement: Linking credential compliance data with quality metrics, patient outcomes, and safety indicators.
When these domains connect through integrated systems—or ideally, live within a unified platform—you gain holistic organizational compliance visibility. Leadership can confidently answer the question "Are we survey-ready today across all domains?"
Implementation action: Map the relationships between employee certifications and other compliance areas in your organization. Identify opportunities to consolidate systems, eliminate duplicate data entry, and create integrated reporting capabilities.
Many healthcare organizations transition from spreadsheet chaos to automated compliance confidence in 6-8 weeks, immediately reducing stress and measurably improving credential compliance rates.
Frequently Asked Questions
What certifications do healthcare organizations typically need to track?
Most healthcare employers must track: state professional licenses (RN, LPN, MD, DO, PA, NP, PT, OT, RT, etc.), national certifications (BLS, ACLS, PALS, NRP, TNCC), specialty credentials (CCRN, CEN, CNOR, OCN, etc.), department-specific competencies, continuing education credits, immunization records (hepatitis B, MMR, varicella, annual influenza, COVID-19, Tdap), tuberculosis screening, respiratory fit testing, and OSHA-mandated training. The exact requirements depend on your facility type, clinical services offered, accreditation standards, and state-specific regulations.
How far in advance should we send expiration reminders to employees?
Healthcare best practices recommend a progressive 90-60-30-15-7 day reminder sequence. The initial 90-day notice provides adequate time for staff to research course options, schedule training around their work commitments, and complete multi-step renewal processes. Subsequent reminders at 60, 30, 15, and 7 days increase urgency and escalate to supervisors and compliance officers. Critical alerts should trigger immediately upon expiration despite all previous reminders, with immediate notification to senior leadership.
Who should be responsible for credential tracking—HR, compliance officers, or department managers?
All three roles share responsibility in an effective system. Individual employees are accountable for completing their own renewals on time. Department managers actively monitor their team's compliance status and follow up on overdue items. HR or dedicated compliance officers oversee organization-wide compliance, ensure policies are followed consistently, generate required reports, maintain audit documentation, and handle escalations. Clear role definitions documented in organizational policy prevent gaps and finger-pointing.
Can we face penalties if an employee's certification expires?
Yes, absolutely. State licensing boards, The Joint Commission, CMS, and other regulatory agencies can issue formal citations, require corrective action plans, and impose significant financial penalties when they discover staff working with expired credentials during surveys or complaint investigations. Serious or repeated violations can escalate to loss of accreditation, deemed status under Medicare, or exclusion from government reimbursement programs. Beyond regulatory penalties, liability exposure increases substantially if a patient incident involves a provider whose credentials had lapsed. According to The Joint Commission's standards, organizations must verify current licensure and certification before granting clinical privileges and at regular intervals thereafter.
What's the most efficient way to store copies of certifications and licenses?
Store high-quality digital copies directly linked to each credential record in your tracking system rather than maintaining separate physical files or disconnected electronic folders. Scan or download PDFs of licenses, course completion certificates, certification cards, and renewal documentation. Use standardized naming conventions (LastName_FirstName_CredentialType_ExpirationDate.pdf) for easy identification. Cloud-based platforms offer secure, instantly accessible storage with automatic backup, version control, comprehensive audit trails, and the ability to produce complete credential files within minutes during surveys. Avoid sole reliance on paper files in cabinets, which are difficult to search, vulnerable to loss or damage, nearly impossible to produce quickly during audits, and create data redundancy challenges.
How do we track certifications for per diem, PRN, temporary, and contract staff?
Per diem, PRN, temporary, and contract staff must meet identical credential requirements as full-time employees if they perform the same clinical duties and have the same patient care responsibilities. Include all non-regular staff in your tracking system from day one of their association with your organization. Set up the same automated reminders and monitor compliance with the same rigor as regular employees. For agency-supplied or contract workers, verify that the staffing agency maintains comprehensive current credentials and request copies of all required documentation for your credential files. Your regulatory compliance responsibility and patient safety obligation don't diminish just because someone isn't a direct W-2 employee—surveyors will hold you accountable for all individuals providing care under your license regardless of employment classification.
Stop the Spreadsheet Scramble: Track Smarter, Stay Compliant, Eliminate Stress
Healthcare best practices for certification tracking share one common foundation: they replace manual, reactive, error-prone processes with automated, proactive, reliable systems that work even when you're not thinking about them.
When you centralize credential records, automate progressive reminders, empower your team with the right purpose-built tools, and establish clear accountability at every level, you transform credential management from a constant source of anxiety into a routine, reliable operation that runs smoothly in the background.
The stakes are genuinely too high—patient safety, regulatory compliance, professional liability, and your facility's reputation—to continue relying on outdated tracking methods. Missed renewals aren't just administrative headaches that create extra work; they're preventable risks you simply can't afford.
Ready to eliminate credential expiration surprises and achieve audit-ready confidence?
Expiration Reminder makes it remarkably simple to track every employee certification, license, training record, and qualification in one secure, HIPAA-compliant platform. Set up fully customized automated reminder sequences specific to each credential type, attach unlimited supporting documents directly to records, generate comprehensive compliance reports with just a few clicks, and give your team self-service access to view their own status. Start your free trial today and discover how healthcare organizations are eliminating compliance stress while protecting patients and their mission.
P.S. A single expired clinical credential can trigger a regulatory violation, force you to pull a provider from the schedule during a staffing crisis, expose your organization to professional liability, or create genuine patient safety risks. But with automated tracking and proactive progressive reminders, those nightmare scenarios become relics of the past. Give your team the visibility, confidence, and peace of mind they deserve—see how Expiration Reminder works in a quick 10-minute demonstration, or start tracking immediately with our free trial. No credit card required.


%20(52).png)

.webp)
.webp)